Get rid of your TMJ Pain without any Surgery
The temporomandibular joint (TMJ) is the joint of the jaw. It acts like a sliding hinge, connecting your jawbone to your skull. The TMJ is a bilateral synovial articulation between the mandible (lower jaw) and the temporal (lower lateral walls of the skull) bone. TMJ disorders or TMD can cause pain in your jaw joint and in the muscles that control jaw movement.
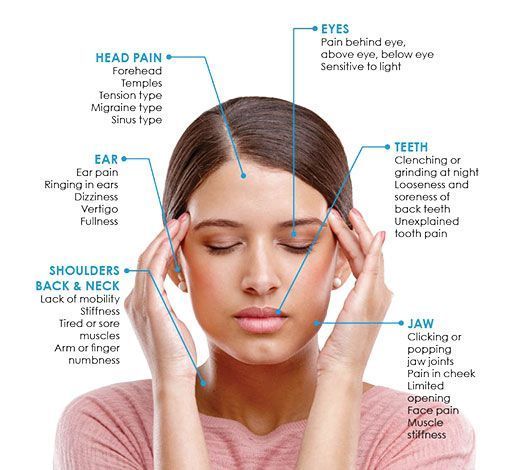
Do you suffer from any of the following ?
There can be a wide number of causes responsible for TMJ disorder. it can be due to irregularly positioned teeth, incorrect relation of the jaws, trauma to the jaws as a result of a fall or an accident, constant grinding of the teeth unknowingly (bruxism), stress, incorrect dentures/crowns/bridges that disrupt the occlusion, arthritis or even genetic.

You must visit a TMJ specialist in kolkata, if you have TMJ disorder symptoms such pain or tenderness in your jaw, or if you can’t open or close your jaw completely. If you are wondering ‘is there a TMJ clinic near me?’, you must visit Dental World as soon as possible for a TMJ treatment consultation and effective Neuromuscular disorder treatment.
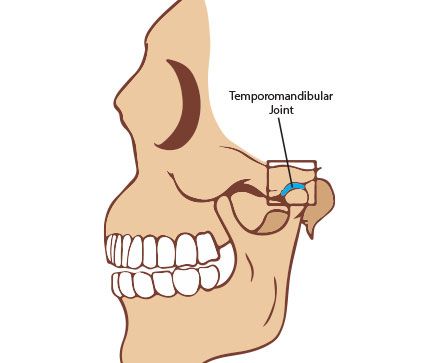
The temporomandibular joint combines a hinge action with sliding motions. The parts of the bones that interact in the joint are covered with cartilage and are separated by a small shock-absorbing disk, which normally keeps the movement smooth.
Painful TMJ disorders can occur if:
Sleep apnea is a sleeping disorder that can lead to serious health problems, such as high blood pressure and heart trouble, if untreated. Untreated sleep apnea causes breathing to stop repeatedly during sleep, causing loud snoring and daytime tiredness, even with a full night’s sleep. Sleep apnea can affect anyone, but most often older men who are overweight.
Most of us know someone who snores during sleep. You may also know someone who has commented that their partner has stopped breathing during sleep for seemingly long periods – long enough to be frightening. While snoring is often made the subject of jokes or teasing, it could be an indication of a serious health problem. sleep apnea symptoms ranges from snoring that irritates your partner to life-threatening medical conditions. If the apnea involves physical obstruction of the upper airway and/or heavy snoring, it is sometimes referred to as Sleep Disordered Breathing (SDB). In this pamphlet we’ll focus on Obstructive Sleep Apnea (OSA) as it is the most common form of sleep apnea.
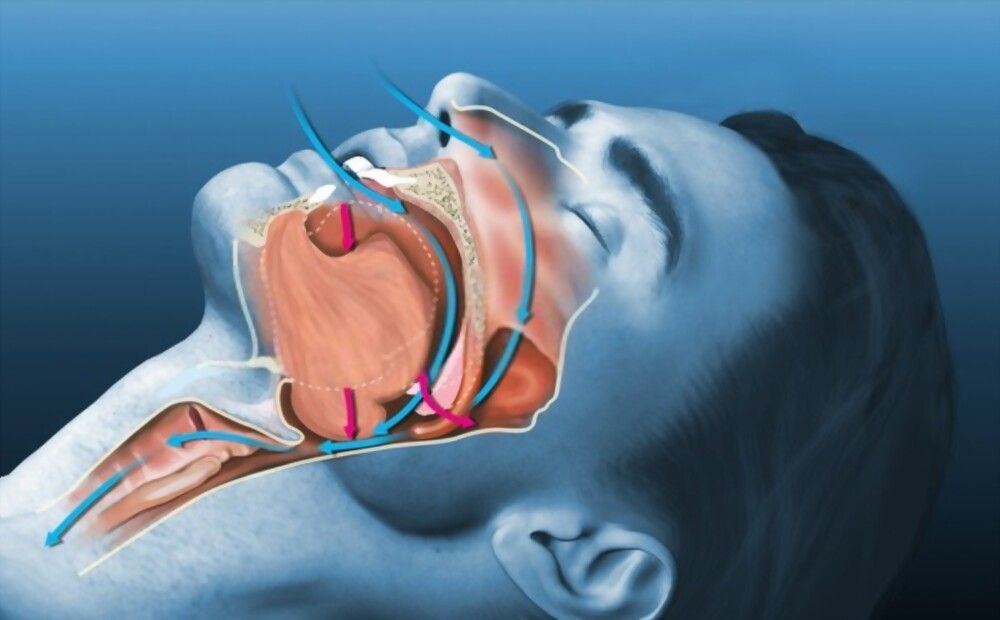
OSA describes an effort to breath, but there is a physical obstruction of the airway causing sleep apnea syndrome. It may be caused by a collapse of the soft tissue at the back of the mouth and in the throat, sometimes related to the inability to properly breathe through your nose. If the jaw is too small to accommodate the tongue, the tongue has a tendency to fall back, further restricting your airway. This constriction impedes airflow. As you inhale and exhale, the soft tissue of the throat vibrates and causes the sound of snoring. This tissue gets flabbier over time. In more severe cases, when apnea occurs - you literally stop breathing for 10 seconds or more. When breathing stops, blood oxygen levels fall forcing the heart to work harder, causing blood pressure to rise. While this may disturb the sleep cycle, the person often does not fully wake up but feels tired in the morning. Some of the conditions associated with Obstructive Sleep Apnea include high blood pressure, obesity, heart disease, gastric reflux, depression, and diabetes. While OSA contributes to these conditions, they in turn worsen OSA, forming a vicious cycle. It is important to note that you don’t have to be overweight to have OSA.
Common sleep apnea symptoms include Snoring, Fatigue, Waking up Tired, Weight Gain, Dry Mouth/Throat, Sleepiness, Difficulty Concentrating, Irritability.
If a young child habitually mouth-breathes or exhibits any of these indications, it is especially important to have them evaluated as these conditions have a significant negative impact on development and form of oral-facial structures. It is also interesting to note that some studies have shown that sleep disordered breathing is common among children diagnosed with Attention Deficit Hyperactivity Disorder (ADHD).
Because of the potentially serious aspects of sleep apnea, you should start with a medical examination and evaluation of your condition. Talk to your dentist who can refer you to a qualified physician with specialized training in the field of sleep medicine. Evaluation can range from an examination of your airway to an overnight sleep study called a Polysomnogram (PSG), followed by treatment that could be in tandem with your dentist.
In some cases, surgery to remove obstructions or to stiffen the flabby throat tissue may be recommended for treatment. For cases of severe sleep apnea, Continuous Positive Airway Pressure (CPAP) is often the first choice for treatment. This means wearing a mask while sleeping that is connected to a small device that maintains a positive air pressure, pushing air into your lungs. However, although painless and effective, some patients and their partners do not tolerate sleeping with CPAP machine very well. In those cases, and in many moderate cases,oral appliances are often a good choice.
Sleep apnea medicine specialist can make custom fitted oral appliances that are worn over the teeth at night to prevent the jaw from falling back during sleep, keeping the airway open. There are many designs of such appliances, and your TMJ specialist will recommend the best one for your sleep apnea treatment.
One of many designs is pictured here as an example. They can be very valuable in moderate cases of OSA or when the patient cannot tolerate CPAP.
If you or someone you know exhibits any of the tmj symptoms listed in this pamphlet, be sure to bring it to our attention. Dental World is the best TMJ treatment clinic in Kolkata and can provide further information for you about this potentially serious condition. You could save a life!
Dental World Super Speciality Clinic has special team for treatment for neuromuscular disorders.Correcting the alignment of jaws and bite of the teeth is the main objective of Neuromuscular dentistry.
Neuromuscular orthodontic techniques that investigate the interrelatedness of the muscles, bones, joints and teeth involved in oral function, hold promise for the treatment of a spectrum of oral disorders. Indeed, such technologies will help patients receive a more targeted level of care. Orthodontic treatment is done for recurrent pain of the temporomandibular joint (TMJ), misaligned teeth, and irregular clicking noises during mouth opening. The basic principles of the use of mandibular tracking, surface electromyography, and transcutaneous electrical nerve stimulation (TENS) to diagnose malocclusions and determine the cranio-mandibular relationship. Neuromuscular orthodontics provides detailed functional analyses through a combination of technologies, by evaluating the needs of the patient thereby delivering treatment. Further deployment of such techniques should, therefore, be encouraged to increase orthodontic health and practice.
The treatment time for neuromuscular orthodontics ranges from 9 to 24 months, depending on how severe of movement is necessary. Our TMJ specialist will guide you thoroughly regarding your Neuromuscular disorder treatment.
Anyone suffering from TMJD needing orthodontics treatment should go for neuromuscular orthodontics treatment. Indeed, neuromuscular orthodontic technologies will help patients receive a more targeted level of care.
Neuromuscular orthodontics work to relax the positioning of the muscles of the upper and lower jaws, which in turn allows for optimal shaping and positioning of each jaw. This translates to greater comfort for the patient, and better, longer lasting results following orthodontic treatment. Again, the goal is to permanently move the teeth into the position that is physiologically correct for your head and neck and posture.
If neuromuscular orthodontics disorder is left untreated, it can contribute to significant discomfort and tension. Chronic pain can even lead to the development of diseases like anxiety and depression.
204, A.J.C. Bose Road, AJC Tower 4th floor, Kolkata – 700017
Ph : +9133 4000 1622 / 4007 5044
Centre for Implant & Aesthetic Dentistry : 204, A.J.C. Bose Road, AJC Towers,
2nd floor, Kolkata – 700017, Ph : +9133 2290 0185
Merlin Metrix, Plot No. 10, Block – DN, Sector – V, Salt Lake City
Ph : +9133 4061 2026